Angioplasty and Stent
Coronary angioplasty procedure
If you have a coronary angioplasty, you will usually have to stay in hospital overnight. Before the operation, you will be asked not to eat or drink anything for about four hours. Before having a coronary angioplasty, you may be given anti-platelet medicine, such clopidgrel, to help prevent blood clots forming in the stent (a device that is often used to widen arteries - see below). You may also be given aspirin (if you are not already taking it) to help thin your blood, and an anticoagulant, such as heparin.
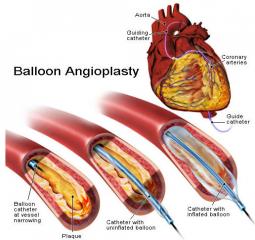
The procedure usually takes 30-60 minutes to perform, but it may take longer depending on how many sections of your artery need to be treated. From a patient’s point of view the procedure is the same as a coronary angiogram. During the procedure, a catheter is inserted through an artery which leads to your heart. The heart specialist will use an X-ray machine to guide the catheter into the right place. A fine wire is the passed through the tube into the artery, and across the narrowed or blocked segment. Once the catheter is in place, another thinner tube with a tiny, deflated balloon on the end is passed through it and into the artery being treated. The balloon is inflated to open the narrowing. A stent mounted on a balloon catheter is then implanted, and squashes the fatty deposits against the artery wall. As the balloon is inflated, the blood flow will be briefly interrupted, and there may be discomfort in the chest. However, this eases when the balloon is deflated, and the procedure is otherwise painless and performed under local anaesthetic.
Before the catheter is removed, an angiogram is carried out to check that the artery has opened up. Once the procedure is complete, a pressure dressing may be applied to you arm, or groin, to help seal the artery. Stitches are not normally required.

Stents
In the past, coronary angioplasties were carried out without using stents. However, 'stenting' has now become a routine procedure and stents are usually used unless the artery being treated is too narrow.
There are several different types of stent. In the UK, the two types of stent that are licensed for use are the bare metal (uncoated) stent and the drug-eluting stent (coated) which is coated with medication that reduces the risk of the artery becoming narrowed again.
The National Institute for Clinical Excellence (NICE) recommends that a bare metal stent should be used to treat short, wide segments of narrowed arteries, and that drug-eluting stents should be used in cases where the arteries are smaller with long segments of narrowing. This is because arteries that are small are more likely to become blocked again and have more benefits from drug eluting stents. Approximately 70% of stents implanted in the UK according to NICE guidelines are drug eluting.
In most cases of coronary angioplasty where the artery is average sized, the number of people who need further treatment is about 1 in 10. For those who have a coronary angioplasty using a drug-eluting stent, about 1 in 10 people will need further treatment for the artery with the stent within a year.
After a coronary angioplasty
In most cases patients are able to leave hospital the day after having a PCI procedure. Patients will be informed about any medication that they need to take, and may receive advice about improving your diet and lifestyle.
Following a coronary angioplasty, there may be a small bruise under the skin where the catheter was inserted. Although this is not serious, it may be sore for a few days. Occasionally, the small wound where the catheter was inserted can become infected. Keep an eye on the wound to check that it is healing properly, and the doctor should be informed if it appears red or swollen.
After the procedure patients should avoid doing any strenuous activity, such as heavy lifting, until after the small wound where the catheter was inserted has healed up. Patients should also avoid driving a car, or a motorcycle, for at least a week after the operation. For those who drive a heavy vehicle, such as a lorry or a bus, they should not drive for at least six weeks. After this time, they should be able to drive again provided that:
· they meet the requirements of an exercise/function test, and
· they do not have any other disqualifying health condition.
Most people do not experience serious problems following a coronary angioplasty, but as with all interventional procedures, there are some risks and possible complications.
Possible side effects
Occasionally, some people have an allergic reaction to the dye that is used to show up the coronary arteries on X-ray. Before having the operation, patients should tell the doctor about any allergies.
Possible serious complications
Serious complications resulting from coronary angioplasty are rare, but do sometimes occur. They are mainly a risk for people who already have serious heart disease. Details of some of the more serious complications are outlined below.
· The artery becomes completely blocked. This occurs in about 1% of cases and to help prevent it, blood thinning anticoagulant medication is often used. However, in some cases, an immediate coronary artery bypass graft may be required to unblock the artery.
· A heart attack during the operation. This occurs in less than 1% of cases.
· The catheter damages the coronary artery. This occurs in less than 0.5% of cases. If it does, the artery may be repaired using emergency heart surgery.
· A stroke may occur during the procedure, but this is also very rare.
It is possible to die as a result of one of the above complications but, again, it is rare for this to happen.
Possible long term problems
Following a coronary angioplasty, it is possible for your coronary arteries to become narrowed or blocked again (restenosis). If this happens, it will usually occur within the first three months after the operation. However, it can happen later than this, but if the artery remains open for a year, the chances of it becoming blocked again are significantly decreased. Re-narrowing of the artery that restricts the blood flow will cause a patient’s angina to return and sometimes may cause a heart attach.
If the coronary arteries do become blocked again, another coronary angioplasty may be recommended, or a different type of treatment, such as coronary artery bypass surgery, may be considered