Electrophysiology
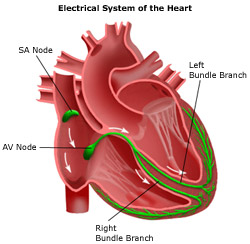
An electrophysiology study (EP study) is a procedure in which a thin tube (catheter) is inserted into a vein or artery (e.g., in the groin) and guided to the heart, where it can perform highly specific measurements of the heart’s electrical activity and pathways. These measurements are particularly helpful in the diagnosis of abnormally fast heart rhythms (tachycardias) or abnormally slow heart rhythms (bradycardias). An EP study is typically performed only after other noninvasive tests, such as an electrocardiogram (EKG), have been performed.
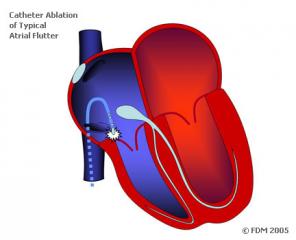
The results of an EP study may lead to further treatment, such as the implantation of a pacemaker or implantable cardioverter defibrillator, or the prescription of antiarrhythmic medications.Because EP studies can pinpoint the source of abnormal electrical conduction rhythms, the physician may decide to perform a catheter ablation. This procedure destroys selected, abnormal areas of the heart’s conduction system, restoring the heart’s normal electrical activity. It is often performed in conjunction with the EP study.
If the physician does not need to do additional procedures (e.g., an ablation) during an EP study, then the patient can go home after about six hours. However, a hospital stay of up to 24 hours is usually necessary if additional treatments are performed during the EP study.
Conditions Diagnosed Using EP Studies
Electrophysiology (EP) studies are used to locate and diagnose the cause of known arrhythmias, whether they occur in the upper chambers of the heart (atria) or lower chambers of the heart (ventricles). In general, EP studies are only recommended for patients whose conditions could not be adequately diagnosed with a standard electrocardiogram (ECG). Because the EP study is invasive, it is not considered a first-line diagnostic test for arrhythmias.
EP studies can diagnose bradycardia–related conditions such as:
- Sinus node dysfunction. The EP study can be used to assess patients with symptoms of sinus node problems that cannot be explained by other tests (e.g., an electrocardiogram, exercise stress test, stress test or tilt-table test.
- AV block. An EP study can be used to diagnose patients in whom an atrioventricular (AV) block is suspected but not confirmed, such as patients with chronic intraventricular conduction delay.
EP studies can also diagnose tachycardia-related conditions, such as:
- Complex tachycardias. An EP study is used to assess those patients with possible narrow or wide QRS complexes (the electrical waves used to measure heart rhythm) whose diagnosis remains unconfirmed after an EKG, who require an assessment of treatment alternatives or in whom drug therapy is unsuccessful.
- Wolff-Parkinson-White syndrome. The EP study may be performed prior to the elimination (ablation) of abnormal electrical conduction in the heart or to gauge the effectiveness of treatments already given.
- Syncope. The EP study can help the physician to diagnose patients whose syncope (fainting) remains unexplained after tilt-table testing and other medical tests.
Furthermore, an EP study may be performed before implantation of a pacemaker. Information from the EP study is used to assist in programming the pacemaker, or after implantation in special situations where performance data cannot be retrieved from the pacemaker itself.
The EP study is also used before implantation of an implantable cardioverter defibrillator (ICD), which is often used to treat abnormally fast heart rhythms. Information from the EP study can assist the physician in selecting the appropriate type of ICD, monitoring progress during the implantation surgery, programming the device and, after the procedure, measuring device effectiveness. EP studies can also assess the effectiveness of antiarrhythmic medications.
The EP study can also determine which patient with syncope or heart dysfunction would likely benefit from placing an ICD for prevention of sudden cardiac death. Patients are considered at higher risk of fatal arrhythmias if arrhythmias (ventricular tachycardia) can be induced by electrical stimulation during EP testing.
EP Studies - Before,During and After the Procedure
Before the day of the electrophysiology (EP) study, patients should discuss their medical history with their physician and inform him or her of any medications currently being taken. Certain medications may need to be discontinued or dosages reduced at some point prior to the test. Also, patients with diabetes are advised to consult with their physician regarding food and insulin intake, because people are generally asked to stop eating and drinking for about six hours before the test.
Just prior to the procedure, the area to receive the electrode catheter is shaved and sterilized to prevent infection. A mild sedative is usually administered.
The EP study may take up to three hours. The patient is first taken to a sterile EP laboratory that resembles an operating room with monitoring devices, video display equipment and x-ray cameras. Once the patient is made comfortable, heart and blood pressure monitoring begin, and an intravenous (I.V.) line is inserted. The area to receive the electrode catheter is then locally anesthetized. The injection of the local anesthesia may result in a brief period of discomfort. This is normal and should be no cause for concern. In fact, this will likely be the most uncomfortable phase of the procedure.
Once the local anesthesia takes effect, the physician will prepare to insert the electrode catheter. Depending on the point of puncture (e.g., the groin), a small incision may be made or a needle may be inserted into a blood vessel. The electrode catheter, which is connected to a computer that will record the data, is then guided with the assistance of an x-ray camera toward and into the heart.
Once in place, the electrode catheter will record electrical activity to assess the presence of abnormal heart rhythms (arrhythmias). The physician may also administer a small electrical shock during the procedure in an attempt to stimulate an arrhythmia.
Depending on what the physician finds, he or she may use the opportunity to perform an ablation while the catheter is still in place. During this procedure, radiofrequency energy is used to destroy selected sections of cardiac tissue that are causing abnormal heart rhythms.
At the conclusion of all procedures, the catheter is withdrawn. Pressure is placed on the point of puncture and, if an incision was made, it will be stitched up (sutured).
After leaving the EP laboratory, patients will remain in bed with their legs straight for several hours. Medical staff will regularly check vital signs, check the point of puncture for swelling or infection, and administer pain medications as necessary. Patients may remain in the hospital for 24 hours for observation. The results of the study may be available before patients leave the hospital, or in the next few days.
Further treatment may include the implantation of a pacemaker or implantable cardioverter defibrillator or a prescription for antiarrhythmic medications.